PET study design
After the tracer has been selected and its radiosynthesis is reliable, and the model has been developed, and validated, the experimental design needs to be optimized, based on previous studies and simulations. Trade-offs between the convenience of the study procedure, the speed of data processing, and the reliability and level of detail of the results are necessary.
Notice also that the best method in science laboratory may not be feasible in clinical laboratory, with limited tracer availability, and requirement for high throughput.
- Avoid acute stress
- Injected dose
- Tracer administration
- Scatter
- Interval of data collection and PET frame times
- Selection of input function
- Blood sampling and metabolite analysis
- Image reconstruction parameters
- Partial volume correction
- Minimization of movement
- Movement correction
- Anatomical reference image
- ROI drawing method
- Parametric mapping
- Constraints in fitting
- Quality system
Avoid acute stress
PET scan can cause acute stress and anxiety, which may have major effect on the results. In repeated studies the stress level is highest during the first scan, causing artefactual results, or add to the variance of results.
Injected dose
Increasing injected dose enhances the quality of PET image, plasma curve, and plasma metabolite analysis, and enables longer imaging. But it also increases the radiation dose (Gy) of the personnel and study subject, limiting the number of PET studies that can be performed for each subject.
If specific activity of the tracer is low, the mass of the radioligand may become a limiting factor for the injected dose, especially when small animals are being studied (Jagoda et al., 2004; Kung & Kung, 2005).
Very high administered doses may lead to saturation of detectors just after tracer injection, especially if heart is in the field of view, and with older PET scanners. Detector dead time may be too high also in blood sample analysis, but that can be solved by letting blood samples decay before measurement.
Tracer administration
In theory, model fitting results will be more accurate with sharper input curve peak, especially when using tracer with fast kinetics, favouring as fast tracer administration as possible.
However, the time resolution of PET scanners in measuring the tissue concentration curves is in the range of a few seconds, and manual blood samples cannot be withdrawn faster than at 10-15 s intervals. Very fast bolus injection may also increase the detector dead-time problem. Therefore, slower tracer infusion may improve the accuracy of the measurements.
Gaseous tracers (for example [15O]O2, [15O]CO, [15O]CO2) may be administered by inhalation. This leads to wider peak in the input function, which is not a problem when analysis is based on the equilibrium state ([15O]CO) or when tracer inhalation is continued to achieve steady state. When faster bolus is required, the gaseous tracers can be mixed with blood and administered normally as intravenous bolus.
If more than one study is conducted to the same subject at one session, it may be advantageous to administer the next dose already before the isotope from the first injection is decayed. These dual- or triple-injection studies not only shorten the scan time, but may even provide more accurate modelling results, if a dedicated compartmental model can incorporate the tissue and input data. Otherwise the background subtraction is required, but it may introduce significant errors to the data.
Constant tracer infusion, or bolus+infusion may sometimes be a method of choice: in case of reversible tissue kinetics a steady state is formed, and analysis of the steady-state data is simple and reliable, and allows studying for example neurotransmitter release during one study session. However, reaching true steady state may be difficult, and radiation dose may limit the study duration. For tracers with irreversible tissue kinetics the constant infusion protocols are usually not applied.
Intraperitoneal, enteral, or retro-orbital administration of [18F]FDG may also be an option in small animal studies.
Try to prevent extravasation when performing venous administration. Minor tracer leakage outside the vein does not affect quantitation, if input function is measured, but will affect SUV.
Scatter
Modern PET scanners have advanced built-in scatter correction methods, but in extreme situations the correction may fail, possibly leading to overcorrection in regions with relatively low radioactivity concentration.
Problems with scatter may arise for example when the tracer is administered via inhalation, and lungs are very close to but not inside the FOV.
Proper shielding may reduce the scatter, but it may be uncomfortable to the study subject, or prevent necessary data acquisition, for example recording subject movement.
PET time frames
Duration of the study
The time window of PET depends on the kinetics of the tracer, as well as what is feasible with the PET scanner and plasma metabolite analysis method.
When the PET tracer is administered as a bolus, in the first phase of the tissue concentration curve we will see the impact from blood in the vascular volume in tissue. This is usually seen only in the first time frames, because concentration in blood decreases with time, and initially the concentration in interstitial and intracellular space of tissue is very low.
Next, the tissue curve is mainly affected by perfusion and transport across endothelium and tissue cell membranes. Most of the tracer then resides in extracellular space and as free tracer in intracellular space.
Then, we will start to see also the effects of specific binding to receptors or enzyme activity, and finally we find out whether the isotope label is trapped inside the cells or if it is released from the cells at some noticeable rate.
In practise, the optimal study duration is determined by conducting a few very long PET studies. After the full length data is analyzed, the data is re-analyzed excluding the late part of the data. When even more data is excluded, the result starts to become biased and standard deviation tends to increase. The optimum study length is where the results still are acceptable. Simulations and bootstrap method can also be used to estimate the effect of study length on the quality of the results.
However, the release or build-up of tissue radioactivity at late times needs not to be due to the original tracer. The labelled isotope may then be attached to another molecule because of some enzymatic process in the liver, kidneys, or the tissue itself. If label-carrying metabolite is missed in the plasma metabolite analysis or not accounted for in the model, the analysis results will be biased, and even more biased if the PET scan time is prolonged.
Analysis methods which require arterial blood sampling generally provide results that are less dependent on the scan duration. Simple semi-quantitative methods like SUV and ratios may still provide meaningful clinical results, but the scan time must be validated: select the scan time that best correlates with the quantitative method, or that best predicts the clinical outcome.
Time frames
The measurement of radioactivity requires a certain time frame, which must be long enough to provide sufficient count statistics. On the other hand, accurate decay correction requires that the concentration of radioligand in the tissue must not change much during the time frame. Therefore the time frames are usually shorter in the beginning when the radioactivity concentration is high and changes rapidly, and longer towards the end of the study when the counting statistics requires longer frames, and the slow concentration changes do not require short frames.
Detailed compartmental model analysis of PET data requires that not only the concentration but also the shape of the tissue TAC is accurately measured, especially if the fast components of tissue uptake are of interest, like in perfusion studies, or if vascular blood volume must be precisely estimated. Delay correction may require short time frames in the beginning, or collecting separate count-rate data.
Graphical analysis methods (Logan, Patlak) do not require short time frames. SUV, FUR and ratio methods can even be applied to late-scan studies with only one long frame.
Modern PET scanners store the data in list mode, which enables us to reconstruct the images with different time frames. However, this procedure is time-consuming, especially if requested long time after the PET scan. Therefore, the final framing should be determined after the first pilot studies.
Selecting input function
Concentration of tracer in arterial plasma as a function of time is the "gold standard" input function. However, blood sampling is uncomfortable to the patient, and adds significantly to the workload for the laboratory technicians.
If absolute quantification is not necessary, then semiquantitative results like SUV can be calculated without input function.
It may be possible to extract the arterial input function from dynamic PET image. For example if the heart is located in the field of view the blood sampling can be replaced with left ventricular blood pool data acquisition. Model-based or population-based input function can be applied to certain tracers and study populations.
In the brain receptor studies, often a region (e.g. cerebellum) exists where specific tracer binding is insignificant and which can be used as reference region; the reference region curve can replace the plasma data in Patlak and Logan plots. Compartmental models with reference tissue input can be used to estimate the binding potential. Reference region can be used also for simple ratio calculations.
Venous blood sampling is less invasive than arterial sampling. If appropriately validated, arterialized venous plasma curve can be used instead of arterial input, or arterial-venous concentration differences can be modelled (Syvänen et al., 2006).
Blood sampling and metabolite analysis
Blood or plasma?
If tracer can pass the red blood cell (RBC) membrane, and if equilibrium between concentrations in RBC and plasma is formed during bloods passage through capillaries, then arterial blood must be used as input instead of plasma.
Compartmental model fitting requires that both plasma and blood TACs are measured, or at least that a method exists for estimating blood TAC from the plasma TAC.
Manual sampling or automatic blood sampler?
Automatic blood sampling system is preferred when the tracer has very fast kinetics (perfusion tracers) or when detailed compartmental models are applied.
However, there are some drawbacks in using the blood sampler: Dispersion and delay in on-line sampling systems can be significant and needs to be corrected. On-line sampler measures tracer concentration in blood, not in plasma. Usually tracer concentrations are different in plasma and blood, and the blood curves must be converted to plasma curves; this is an additional source of error, compared to manual plasma sampling. With many tracers the blood-to-plasma ratio changes with time, and therefore separate blood and plasma samples must be collected during the on-line sampling to measure a correction factor function. And further, if plasma curve needs to be corrected for metabolites, then separate samples for parent fraction determination need to be collected even during the on-line sampling.
Blood sampling schedule
Rule of thumb: one blood/plasma sample at the middle of each PET frame. If PET time frames are more frequent than plasma sampling, then Patlak and Logan plots may look strange, and the gaps need to be interpolated by fitting function to the plasma TAC.
Most important is to measure accurately the AUC of the input TAC. Also the shape of the peak is important in compartmental model fitting. Manual samples can be taken in 10-12 s intervals, and if more frequent sampling is needed, then automatic blood sampling system must be used. If delay correction is needed, then the ascending part of the input curve must be accurately measured.
Because of the time delay the plasma TAC usually starts to ascend 20-50 s after the tracer administration. It is still necessary to collect samples towards the end of this period; otherwise the AUC of the initial part cannot be correctly calculated. Also if the initial part of blood TAC is taken from dynamic PET image, care must be taken that the ascending part of the blood curve is not missed by starting the PET scan too late.
Notice that plasma sampling schedule must be given to laboratory technicians in good time before starting the PET study, because the blood tubes must be weighed and numbered beforehand.
Is metabolite analysis necessary?
In the most common PET studies, FDG and radiowater studies, this is not needed: there are no labelled metabolites in the plasma during the PET study.
If labelled metabolite appears in plasma during the PET scan, the parent fraction has to be measured and corrected, because the concentration of parent tracer in plasma is the input function for the models. In animal studies a population average of the fraction curve may be used, if treatment does affect the rate whole body metabolism or clearance of the tracer.
Schedule of plasma samples for metabolite analysis depends on the rate of metabolism. Usually no metabolites appear in plasma before 1-3 minutes p.i., and during that time collection of metabolite samples is not necessary. After that the fraction of metabolites usually increases rapidly, and samples should be taken at about 5 min intervals. Note that if too many or too frequent samples are taken, the samples may need to wait longer to be processed, which may impair the reliability of the fractions. In any case, remember to place the metabolite samples immediately in ice to prevent further metabolism and plasma-RBC transport in the sample.
Measurement of fraction of parent tracer in plasma with HPLC and even with TLC may be impossible in the late samples, if the total radioactivity of blood is too low. This may result in an erroneous tail of the metabolite corrected plasma TAC, which would then lead to biased model parameter estimates (Lammertsma, 2002). The error are avoided by using reference tissue input, when applicable. However, that is not an option, if there is uptake of labelled metabolite in the reference region.
An appropriate function is fitted to the measured parent fractions before metabolite correction to allow interpolation and, if necessary, extrapolation of the parent fractions.
Image reconstruction parameters
There are many options for image reconstruction, and it is useful to test what method and which parameters provide the best image quality for this tracer, target organ, scanner, and selected framing schedule.
Image reconstruction may take a lot of computer time, and attempt to speed up the process may lead to reduced contrast in the image, especially in those image frames where the count statistics are poor or the contrast should be high (Johansson et al, 2007). Strong filtering may enhance visual image quality but may lead to increased partial volume effect, and bias in image-derived input function (Boellaard et al., 2001).
If dynamic image is further modelled to a parametric image to be analyzed in SPM, which requires strong smoothing, it may be useful to use strong filtering already in the reconstruction.
Partial volume correction
Partial volume correction would enhance the image contrast but it will also increase the noise. Traditional PVC methods rely on anatomical reference image and assumptions of uniform tracer uptake inside the same anatomical region, which may cause artificially nice looking images.
PSF reconstruction and other contrast enhancing methods inside image reconstruction methods are included in the software of modern scanners. Image-derived blood curve should be validated with blood sampling, since it is common that these methods cause bias in vessel activity concentrations.
Minimization of movement
Movement during the PET study may cause spurious results and even lead to wrong diagnosis, if left unnoticed. Therefore different fixation equipment have been developed. Problem is that restricting movement may be uncomfortable for the study subject, and especially for old patients.
Fixation system must not interfere with MR, if PET-MR is used. It must also not prevent the study subject from doing any tasks that may be part of brain activation or exercise studies.
Movement correction
Movement during the PET scan cannot be prevented, although it can be minimized. If movement is recorded, there are methods under development for correcting the movement effect in list mode data. Easier method is to observe the time points where the movement occurred, re-frame the image, and then correct the movement frame-by-frame. Another option is to use anatomical reference image as a basis of frame-by-frame movement correction.
Notice that movement correction must be done before attenuation correction.
Anatomical reference image
Anatomical reference image is needed for defining regions-of-interest, for movement correction, and to align images to a common template for SPM analysis. CT image may be available when PET/CT is used, but CT may lead to additional radiation dose. MR is usually preferred. CT or MR image that is used for attenuation correction may not be of sufficient quality to be used as reference image.
Anatomical reference image for other than brain studies is usually difficult to obtain, because the body shape is different in the different beds used in different scanners.
ROI drawing method
Regions-of-interest are usually drawn to anatomical reference image and then copied to the summed or parametric PET image for visual inspection, and ROI positions may then be refined if the alignment between PET and reference image was not optimal. ROIs could also be drawn directly to the summed or parametric PET image, but that may less objective method than using the anatomical reference image.
If the tracer is used in more than just a few brain studies, it will be useful to draw template ROIs and use an auto-ROI method based automatic image alignment and anatomical reference images.
Parametric mapping
Most analysis methods can be used to compute parametric images, i.e. applied to each voxel in the dynamic image, producing a functional image where each voxel value represents the parameter of interest, such as binding potential, Ki, or perfusion. Parametric images can be used in SPM, and those can also be valuable in defining ROIs.
Calculation of parametric images is usually sensitive to the noise in the original dynamic image. Noise may cause a skewed distribution of parameter values inside a region, and therefore cause bias in ROI mean values. Therefore strong filtering in the image reconstruction is recommended. Simplified models, such as SRTM, that are usually used to produce parametric images may also introduce bias.
Constraints in fitting
In case of noisy data, and especially in calculation of parametric images, some constraints have to be introduced to the model parameters to enhance the quality of the resulting image and to remove outliers.
However, too tight constraints may force the results to certain direction and prevent us from observing true effects. A notorious example is the basis function method with SRTM: user has to define a range of basis functions, and if the range is too wide, then the resulting parametric binding potential image will be noisy and regional averages biased because of the noise; if the range is too tight, then the binding potential image will look nice, but regions with high or low binding potential may be biased.
Quality system
- When starting new study project, check what is the current analysis method and most recent software versions; do not trust old unofficial "recipes"!
- Follow instructions in our quality system; if not available or out-of-date, then write or rewrite the instructions.
- Follow international guidelines, if available.
Document all analysis steps for each study. Use the same analysis chain and computer program versions for all subjects in one study; these must be defined in study plan, or at least in the report. If new software version appears, recalculate all or nothing. Use analysis pipelines or scripts as much as possible: those work as documentation as such, and allow easy recalculation.
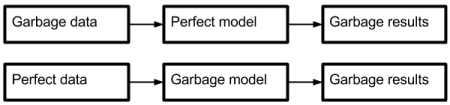
"Garbage in - garbage out" paradigm
See also:
Literature
European Nuclear Medicine Guide
https://www.eanm.org/publicpress/european-nuclear-medicine-guide/
Boellaard R, van Lingen A, Lammertsma AA. Experimental and clinical evaluation of iterative reconstruction (OSEM) in dynamic PET: quantitative characteristics and effects on kinetic modeling. J Nucl Med. 2001; 42(5): 808-817. PMID: 11337581.
Boellaard R. Standards for PET image acquisition and quantitative data analysis. J Nucl Med. 2009; 50(Suppl 1): 11S-20S. doi: 10.2967/jnumed.108.057182.
Glaudemans AWJM, Medema J, van Zanten AK, Dierckx RAJO, Ahaus CTB (eds.): Quality in Nuclear Medicine. Springer, 2017, ISBN 978-3-319-33531-5. doi: 10.1007/978-3-319-33531-5.
Hartung-Knemeyer V, Beiderwellen KJ, Buchbender C, Kuehl H, Lauenstein TC, Bockisch A, Poeppel TD. Optimizing positron emission tomography image acquisition protocols in integrated positron emission tomography/magnetic resonance imaging. Invest Radiol. 2013; 48: 290-294. doi: 10.1097/RLI.0b013e3182823695.
Jagoda EM, Vaquero JJ, Seidel J, Green MV, Eckelman WC. Experimental assessment of mass effects in the rat: implications for small animal PET imaging. Nucl Med Biol. 2004;31:771-779. doi: 10.1016/j.nucmedbio.2004.04.003.
Jones RT. Clinical and behavioral considerations in emission tomography study design. NIDA Research Monograph 74, 1986; 117-125. PDF.
Kagadis GC, Ford NL, Karnabatidis DN, Loudos GK (eds.): Handbook of Small Animal Imaging: Preclinical Imaging, Therapy, and Applications. CRC Press, 2016, ISBN 978-1-4665-5569-3
Kiessling F, Pichler BJ, Hauff P (eds.): Small Animal Imaging - Basics and Practical Guide, 2nd ed., Springer, 2017. doi: 10.1007/978-3-319-42202-2.
Lammertsma AA. Radioligand studies: imaging and quantitative analysis. Eur Neuropsychopharmacol. 2002; 12: 513-516. doi: 10.1016/S0924-977X(02)00100-1.
Piel M, Vernaleken I, Rösch F. Positron emission tomography in CNS drug discovery and drug monitoring. J Med Chem. 2014; 57: 9232-9258. doi: 10.1021/jm5001858.
Svensson JE, Schain M, Knudsen GM, Ogden RT, Plavén-Sigray P. Early stopping in clinical PET studies: How to reduce expense and exposure. J Cereb Blood Flow Metab. 2021; 41(11): 2805-2819. doi: 10.1177/0271678X211017796.
Tags: Modeling, Analysis, Administration, Input function, Image reconstruction, Time frame
Updated at: 2022-01-22
Created at: 2011-11-22
Written by: Vesa Oikonen